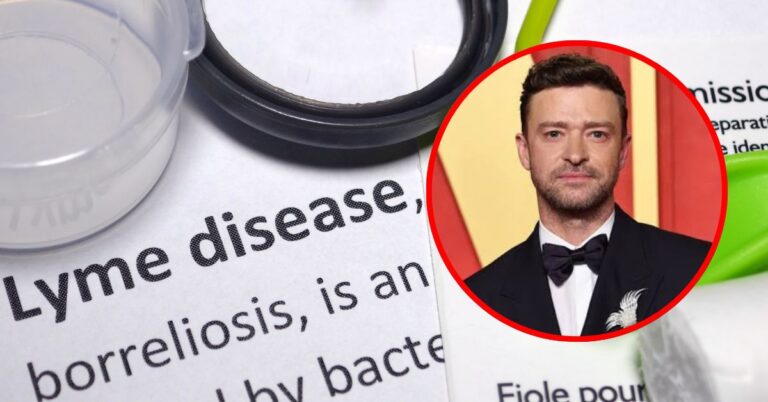
Why Lyme Disease Is Often Misdiagnosed
It all starts with feeling tired. Maybe your joints are aching, or you have a headache that won’t stop. You go to the doctor and get a diagnosis of the flu, chronic fatigue syndrome, or even depression.
But weeks later, the symptoms haven’t gone away and they’ve actually gotten worse. If this sounds like you, Lyme disease could be the sneaky culprit.
Lyme disease is a serious public health issue, even though people are becoming more aware of it. Experts say that the condition is often overlooked, misclassified, or misunderstood, which can delay proper treatment and lead to long-term health problems.
“Lyme disease can look like many other illnesses,” says Dr. Monica Shoff, MD, an infectious disease specialist at the Mayo Clinic.
Why Is Lyme Disease So Often Misdiagnosed?
Lyme disease, caused by a tiny germ called Borrelia burgdorferi, is spread by black-legged ticks. It can cause a variety of symptoms that are similar to other illnesses.
Symptoms often mistaken for:
- Flu or COVID-19 (fatigue, fever, chills, headache)
- Rheumatoid arthritis (joint pain, stiffness)
- Fibromyalgia (widespread pain, fatigue)
- Multiple sclerosis (numbness, neurological issues)
- Depression or anxiety (brain fog, mood changes)
One key issue is the absence of a classic bullseye rash, which only occurs in 70–80% of cases, according to the CDC. Many patients also don’t recall being bitten by a tick, especially since nymph ticks are tiny and painless.
“Lyme disease can be hard to spot because it’s not always on people’s minds in certain areas or times of the year,” says Dr. Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security.
What the Research Says About Misdiagnosis Rates
A study published in BMJ Open in 2024 revealed that a whopping 61% of Lyme disease patients had been misdiagnosed before they finally got the right one. And guess what?
Another study in Frontiers in Medicine found that when Lyme is delayed, those pesky symptoms like fatigue, joint pain, and neurological issues can stick around even after taking antibiotics.
This phenomenon, commonly referred to as Post-Treatment Lyme Disease Syndrome (PTLDS), can persist for months to even years, particularly in cases of delayed diagnosis.
Dr. Shoff emphasizes that early detection of Lyme disease is highly treatable, while prolonged undiagnosis leads to a more complex and challenging condition.
Public Health Impact: A Growing Epidemic
The CDC estimates that nearly 476,000 Americans are diagnosed and treated for Lyme each year but many believe this number is still far too low due to widespread underreporting and misdiagnosis (CDC Lyme Statistics).
In the UK, the National Institute for Health and Care Excellence (NICE) issued new guidelines in response to rising Lyme disease cases and misdiagnosis concerns, urging doctors to consider Lyme even without a rash or known tick bite (NHS Lyme Resources).
Lyme disease is spreading to new areas, partly because of climate change. Doctors in cities or places that weren’t usually at risk might not even think to test for Lyme.
What You Should Ask Your Doctor
If you think you might have Lyme disease or if you’ve been feeling strange for weeks, don’t be afraid to speak up. Here are some important questions to ask your doctor:
Important questions to ask:
- “Could this be Lyme disease, even if I don’t remember a tick bite?”
- “Is a two-tiered Lyme test appropriate right now?”
- “If my test is negative, but I still have symptoms, what’s the next step?”
- “Can I start antibiotics based on clinical symptoms alone?”
- “Could this be Post-Treatment Lyme Disease Syndrome?”
Read more: CDC’s Guide on Lyme Diagnosis and Testing
“Lyme disease can strike anyone, even if you’re not an outdoor enthusiast. If you’re experiencing persistent, unexplained symptoms, it’s worth checking out,” advises Dr. Adalja.
Actionable Advice: What to Do If You Suspect Lyme
If you think you’ve been misdiagnosed:
- Keep a symptom journal with dates, patterns, and photos of rashes if present
- Get a second opinion, ideally from an infectious disease specialist or Lyme-literate doctor
- Ask for a Western blot test, especially if symptoms persist after a negative ELISA
- Explore tick exposure, even if indirect—via pets, gardening, or hiking
- Don’t delay treatment—the sooner antibiotics are started, the better the outcome
See: Mayo Clinic’s Lyme Treatment Protocols
Be Proactive, Not Passive
Lyme disease misdiagnosis is a serious issue that’s on the rise, not because doctors aren’t trying, but because the condition is tricky, unpredictable, and easy to miss. But with awareness, advocacy, and the right questions, you can increase your chances of getting an accurate diagnosis.
“Patients need to feel confident in asking for answers,” says Dr. Shoff. “The earlier Lyme disease is diagnosed, the easier it is to treat and the less likely it is to become a lifelong struggle.”
Check out the healthlynic ✔️approved range of products for Weight Loss, Improve metabolism and much more!